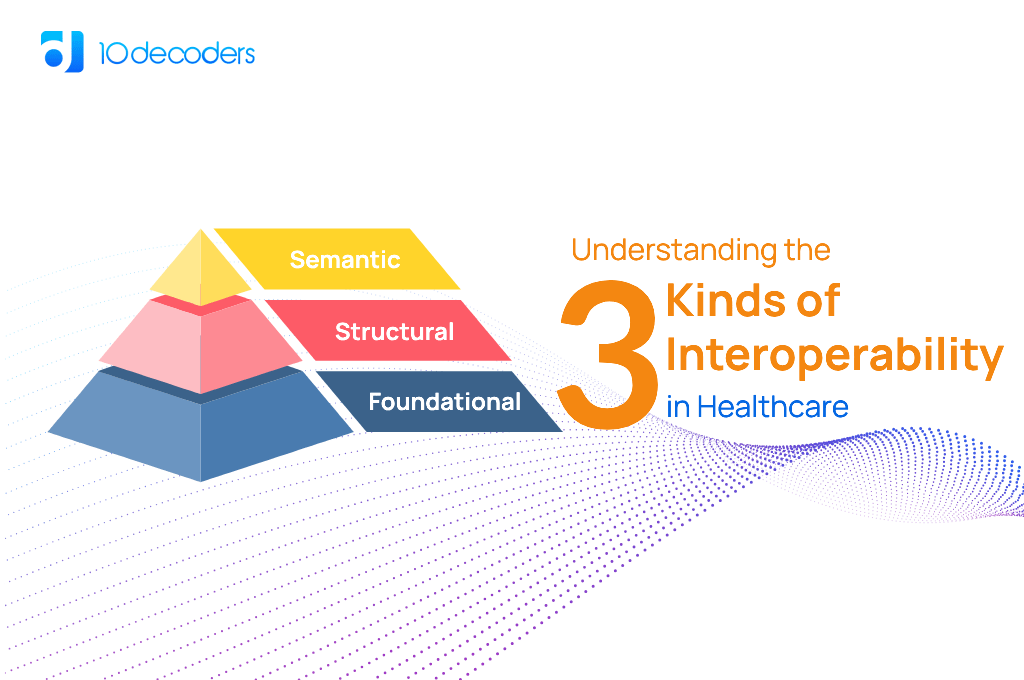
Understanding the Three Kinds of Interoperability in Healthcare
The seamless integration of healthcare IT systems is a pivotal aspect of modern medical care. Central to this integration is the concept of interoperability, which is broadly categorized into foundational, structural, and semantic. Each type plays a unique role in enhancing the efficiency and effectiveness of healthcare delivery. This blog provides an in-depth look at these three types of interoperability, exploring their individual functions and collective importance in the healthcare sector.
Foundational Interoperability: The Gateway to Communication
At its core, foundational interoperability is about establishing a basic level of communication between different IT systems in healthcare. It facilitates the simple exchange of data, enabling systems to send and receive information without necessarily interpreting it.
The Role of Foundational Interoperability in Healthcare
This level of interoperability is vital for ensuring that patient information is transferable across diverse platforms, such as electronic health records (EHRs), laboratory information systems, and radiology systems. It’s the first step in creating a connected healthcare environment, crucial for coordinating patient care and streamlining clinical workflows.
Structural Interoperability: The Key to Organized Information
Structural interoperability goes beyond basic data exchange. It ensures that data exchanged between systems is not only sent and received but also structured in a universally understandable format. This aspect of interoperability focuses on the organization and format of data exchange.
Its Impact on Healthcare Efficiency
In practical terms, structural interoperability enables healthcare providers to interpret and use the information quickly and accurately. For instance, when a physician receives laboratory results or imaging reports, structural interoperability ensures that these are presented in a familiar and organized manner, enabling immediate assessment and timely decision-making.
Semantic Interoperability: The Peak of Data Synergy
The Essence of Semantic Interoperability
Semantic interoperability represents the most sophisticated level of data exchange. It’s not just about exchanging or structuring data but ensuring that the information is interpreted and used meaningfully and consistently across different systems. This requires common data standards and terminologies.
Transforming Patient Care with Semantic Interoperability
In the healthcare context, semantic interoperability is essential for comprehensive and coordinated patient care. It facilitates the accurate interpretation of patient data across various healthcare settings, ensuring that all care providers have a unified understanding of a patient’s medical history, treatment plans, and health outcomes. This level of interoperability is particularly crucial in managing chronic diseases, where continuous monitoring and coordination between different specialists are key.
Bridging the Gaps: Challenges in Achieving Interoperability
Overcoming Obstacles in Interoperability
Despite its clear benefits, achieving interoperability in healthcare is laden with challenges. These include the need for substantial investments in IT infrastructure, the complexity of aligning various stakeholders on standard protocols, and the ongoing concerns regarding data security and patient privacy.
Collaborative Efforts for a Unified Future
The future of interoperability requires a collective effort among healthcare providers, IT professionals, and policymakers. It involves not only the adoption of technological solutions but also the commitment to maintaining the highest standards of data privacy and security. The aim is to create an interconnected healthcare ecosystem that optimizes patient care while safeguarding sensitive information.
The Practical Implications and Future Developments in Healthcare Interoperability
The practical implications of advancing interoperability in healthcare are immense. Enhanced interoperability not only streamlines clinical workflows but also significantly improves patient outcomes. For instance, in emergency care scenarios, the ability of systems to seamlessly exchange and interpret patient data can be the difference between life and death. Rapid access to a patient’s medical history, allergies, and current medications allows emergency teams to make informed decisions quickly. Looking towards the future, the integration of Artificial Intelligence (AI) and Internet of Medical Things (IoMT) with interoperable systems is set to revolutionize healthcare delivery. AI algorithms can analyze interoperable data to provide predictive insights for personalized patient care, while IoMT devices can offer real-time patient monitoring, sending crucial health data to various interconnected healthcare platforms. However, the path to this future is lined with challenges, including the need for widespread adoption of standardized data formats and the integration of legacy systems into modern interoperable frameworks. Addressing these challenges requires not just technological solutions but a shift in the mindset towards a more collaborative and patient-centric approach in healthcare. Embracing this change will pave the way for a healthcare system that is not only more efficient and cost-effective but also more responsive to the needs of patients.
In conclusion, understanding and implementing the three kinds of interoperability in healthcare – foundational, structural, and semantic – is more than a technological endeavor; it’s a step towards transforming patient care. These interoperability levels together create a robust framework for efficient, accurate, and holistic healthcare delivery. As the sector continues to evolve with technological advancements, the focus on improving interoperability will play a crucial role in shaping the future of healthcare, making it more connected, efficient, and patient-centric.